A Proposed Framework Could Help Asia Deal with an Ebola Outbreak
Please note that we are not authorised to provide any investment advice. The content on this page is for information purposes only.
Southeast Asia is no stranger to epidemics and is a hotspot for emerging disease threats. There have been serious economic and health-sector impacts from zoonoses including Nipah virus infections, SARS and highly pathogenic avian influenza (commonly known as bird flu). While these events catalysed some change in infectious disease policies within the region, many countries’ interest has since waned. Many governments, faced with numerous other pressing health priorities, have classified the threat of other emergencies as remote.
Southeast Asia is no stranger to epidemics and is a hotspot for emerging disease threats. There have been serious economic and health-sector impacts from zoonoses including Nipah virus infections, SARS and highly pathogenic avian influenza (commonly known as bird flu). While these events catalysed some change in infectious disease policies within the region, many countries’ interest has since waned. Many governments, faced with numerous other pressing health priorities, have classified the threat of other emergencies as remote.
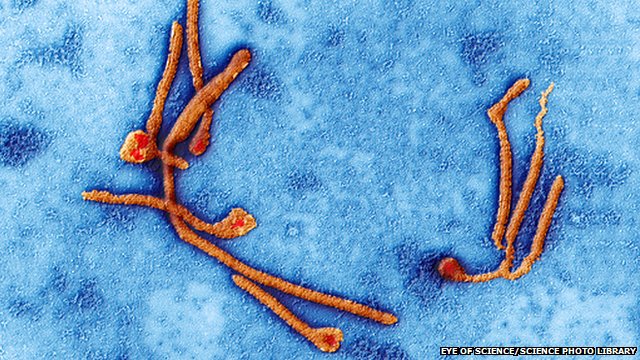
But the recent emergence of Ebola Virus Disease (EVD) in West Africa has laid bare fragilities within international health responses on a global scale, even in countries — such as the US and Spain — where it was previously unthinkable that secondary transmission could occur within health facilities.
A new framework is necessary to assess the risk of an EVD outbreak occurring within a country if a case crosses its borders, and to act as a guide on how to increase country-level preparedness. The framework, which builds on a rapid assessment toolkit for communicable diseases, is designed to highlight that the effectiveness of a country’s response to an outbreak is dependent on a combination of broad factors related to the political environment, health system and local population, as well as on targeted disease-specific measures to prevent the disease from spreading.
The current effectiveness of the health system depends on its capacity to serve the population, including hard-to-reach groups, as well its capacity (in terms of human resources, information systems and laboratories for example) to respond appropriately to a sudden increase in workload.
When formulating general policies for EVD control, local traditions and beliefs about death and disease are often overlooked. There are important variations in religion and culture across countries and within countries in the region. Practices related to burial or cremation, washing of bodies, storage of bodies and community handling of severely ill individuals influences the potential for the spread of EVD. There has previously been a well-founded call to understand and benefit from religious teachings to help curtail transmission in Muslim-majority African countries. Specifically, the use of Islamic guidance on avoiding travel to epidemic-affected regions, and suspending traditions around washing corpses before burial, could help limit the spread of Ebola. Such approaches can and should be applied in Asia, where appropriate and feasible.
Similarly, the level of trust between public institutions and the population is an important determinant of how effective screening, contact tracing and isolation of high-risk individuals may work in a specific countries and communities. Communities or regions in which the reach of the formal health system and institutional trust is low will be at an inherently higher risk of an outbreak as control measures are likely to be implemented slower and less effectively.
In the case of EBV, the formation of a high-level preparedness committee is essential in all countries. This committee, whose mandate should include setting policies and protocols at the national level, should include a broad set of actors with expertise in medicine, public health, transport and mass media.
Also, countries should form a complementary and specially trained medical response team that is on call around the clock to attend to the first reported cases or any high-risk suspects. This team should be comprised of doctors, nurses and laboratory technicians who, as well as being trained to respond, are aware of the risks they are taking on in handling potential Ebola-infected cases.
The risk of transmission to healthcare workers is substantial even with high levels of personal protective equipment. And it will be even higher when necessary infection control measures are not in place owing to general weaknesses in the health system. To date more than 400 healthcare workers have been infected in West Africa and over half of these have died. This tragedy should not be repeated in other resource-limited settings.
Even if this framework was implemented, the process is not without challenges. Preparedness assessments require input from a broad range of technical experts. And countries that are likely to be least prepared are least likely to have preparedness committees in place to raise alarms and ask for assistance. Preparedness is unlikely to be uniform across a country; it may vary due to health system strength, differences in cultural practices, transport links and other local dynamics. Steps to improve preparedness must also strike a delicate balance between information sharing for preparedness and creating panic.
Looking forward, there should be concrete planning at the regional level, to assist country-level committees. In addition, real, transparent dialogue is desperately needed to determine what the global and regional public health community’s role should be in supporting countries with limited capacity for comprehensive surge or preparedness plans. From a regional institutional perspective, these discussions need to ask whether ASEAN has a role and what the World Health Organisation’s regional and country offices’ roles are in supporting preparedness. The Ebola Virus Disease outbreak raises serious questions about the effectiveness of international health regulations.
How can Southeast Asia increase its preparedness for an Ebola outbreak? is republished with permission from East Asia Forum